Technology Plays Key Role in Patient-Centered Room of the Future
// By Sheryl S. Jackson //
 How do you build the children’s hospital of the future? Start by asking family members, patients, clinicians, and other healthcare providers what they want. That is exactly what MUSC Health did when designing MUSC’s new Shawn Jenkins Children’s Hospital set to open in October 2019.
How do you build the children’s hospital of the future? Start by asking family members, patients, clinicians, and other healthcare providers what they want. That is exactly what MUSC Health did when designing MUSC’s new Shawn Jenkins Children’s Hospital set to open in October 2019.
More than 20 different committees comprising hospital staff, physicians, nurses, and family members of patients identified features that would make patients and their families feel comfortable, safe, and confident about care they receive in South Carolina’s only pediatric hospital.
Incorporating those features along with clinical care staff needed to optimize care, and required more than just a different building design, but also required different approaches to communication among patients, families, and hospital staff, as well as technology that supports a higher level of engagement.
One example is MUSC’s transformation of the neonatal intensive care unit (NICU) experience at Shawn Jenkins Children’s Hospital to better meet the needs of infants and families already under severe stress.

Brett Seyfried, associate CIO, infrastructure at MUSC Health
NICU of the Future
“Based on input from family members, we realized that the neonatal intensive care unit (NICU) had to be designed differently,” says Brett Seyfried, associate CIO, infrastructure at MUSC Health. The existing NICU has 66 bassinets in an open room, but the new NICU will have 82 individual rooms for each infant with space for family to stay with the baby.
“Parents wanted the ability to talk or sing to their baby, or talk to each other, without disrupting other parents with their babies,” he explains.
Healthcare provider concerns about the ability to easily communicate with parents and monitor babies was addressed with communication strategies supported by technology that allows parents to easily communicate with providers and sends alerts to nurses when needed.
No More Whiteboard
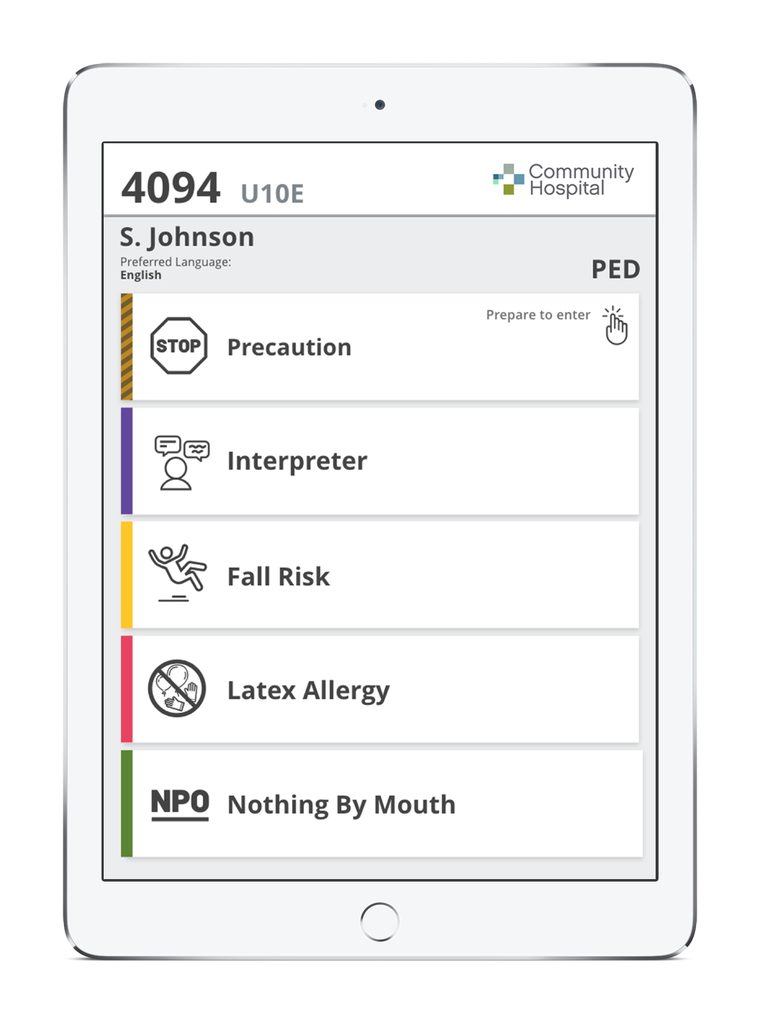
The presence of forward-looking technology will be apparent before the room is entered. A flush-mounted iPad is mounted on the exterior of each patient room and digitally displays the patient name, names of care team members, and any precautions that caregivers must know before entering the room — for example, fall risk or allergies.
“Precautions are indicated by icons that display more detailed information or instructions specific to the patient,” explains Seyfried. “This replaces the whiteboard sign that is handwritten and precaution flags that are typically used.”
Display-Enabled Consults
As care team members enter the room, a real-time location system (RTLS) that operates as part of the identification badge enables the display of the person’s name and role on the care team. “The system automatically displays relevant clinical information, so the provider does not have to log in to the system and pull up a chart,” says Seyfried.
Each patient and clinician has an iPad that can be used to review information, but when multiple family members are present, the clinician can cast the display to the Apple television in the room for a more collaborative discussion. “There is also a camera above the television so a physician can call into the room for a video consultation or attend rounds on patients,” Seyfried says.
Connected Technology

Robin Cavanaugh, chief technology officer at GetWellNetwork
Bedside technology and the use of laptops and tablets has been around for years, but MUSC Health is relying on technology from GetWellNetwork to enable the patient room of the future in the new facility.
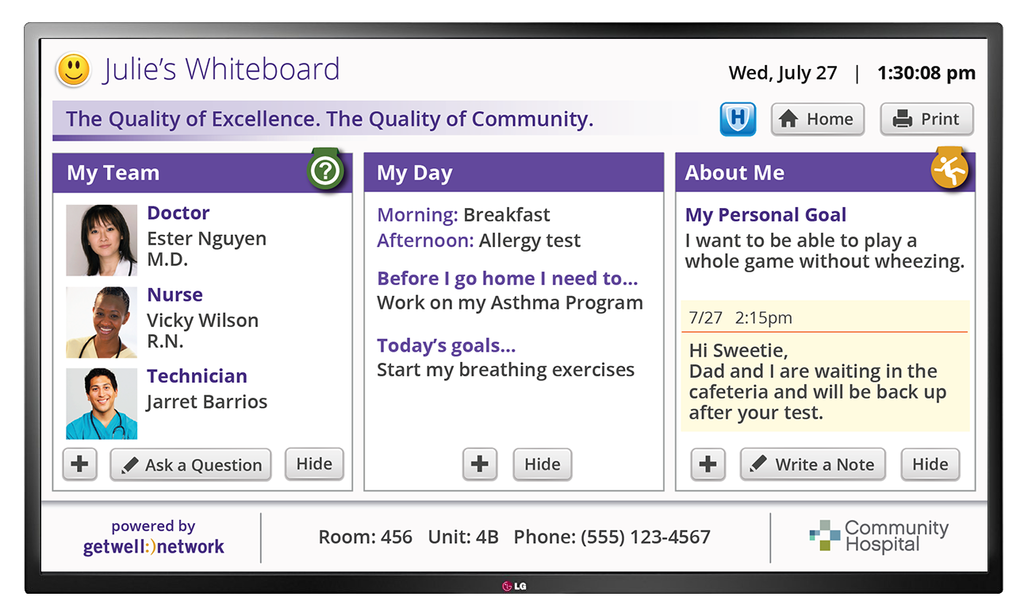
GetWellNetwork offers a number of solutions that can simplify tasks such as documentation, measuring engagement, or obtaining real-time feedback. But the platform also can be used to integrate other systems and applications such as the EMR or a room’s lighting controls.
“It is possible to connect all of the different technologies so that the patient only has to use one device to control the television or lights, connect with a nurse or housekeeping, or review educational materials,” says Robin Cavanaugh, chief technology officer at GetWellNetwork.
He describes a health facility that purchased 85-inch televisions for all patient rooms, which at first glance seems excessive. “When a provider walks into the room, the bottom few inches of the television screen displays the provider’s name, vital stats on the patient, precautions such as allergies and other critical information,” he says. “This hospital was able to avoid purchase of other hardware by leveraging the technology that was already there.”
Because each hospital or medical clinic has different needs, Cavanaugh points out that the first step is to identify critical goals. “One hospital might want to address a high fall rate, so we can set up the system to display a message on the television or iPad reminding the patient to call the nurse before getting out of bed,” he says. “In another hospital, we might choose applications that improve response to pain management or that focus on patient education.”
The key to success is to choose the right applications and tools to meet goals as opposed to implementing technology for technology’s sake, he adds.
Improvements in Efficiency
In use at more than 500 hospitals in the United States, GetWellNetwork is producing positive, measurable results, says Cavanaugh. A few highlights from other health organizations include:
- 66 percent increase in medication education utilization correlating with a 16.4 percent improvement in patient satisfaction with medication at a Bethesda, Maryland teaching health system
- 110 percent increase in HCAHPS scores for environment of care at a 116-bed regional referral center
- 31.2 percent variance increase for overall hospital rating at a Virginia health system
- 17 percent increase in HCAHPS scores for staff responsiveness over a one-year period at an Idaho healthcare facility
- 10-point improvement (14 percent) in pain management HCAHPS scores in just one year at a healthcare facility in the greater Cincinnati region
- 56 percent reduction in hospital falls in one year for a Virginia health system
- 50 percent decrease in hospital-acquired infections at an Eastern health system
- 11,079 nursing hours saved across all hospitals throughout a health system in Kentucky
The real value of seamlessly integrated technology is the ability for collaboration, even if a physician is not at the hospital, points out Seyfried. “If a child with sickle cell is in the hospital, but the physician who regularly provides care is not on-site, the physician can call into the room, see the patient, and discuss treatment with the family, child, and hospitalist,” he says. “It all takes place with one conversation, which can improve the speed of response, which is likely to improve the outcome.”
Sheryl S. Jackson is a writer and editor specializing in marketing, leadership and management topics for the healthcare, education, construction, and supply chain industries. You can reach her at sherylsjackson@bellsouth.net.