Predictive Analytics Platform Optimizes OR Utilization at Boston Medical Center, Improves Bottom Line
// By Jane Weber Brubaker //

Rich Krueger, CEO and Founder, Hospital IQ
Hospitals today are coping with severe financial pressures driven by cuts in reimbursement, penalties, and the shift from fee-for-service to value-based models. One company is helping health systems drive out waste and improve efficiency by applying operations management and quality improvement principles developed and refined in manufacturing. “There’s a lot of great work that’s been done by consultants and academics in applying operations management principles to the delivery of care, but no one has built a system to make it easy to consume,” says Rich Krueger, CEO and Founder of Newton, Massachusetts-based Hospital IQ.
Yi-An Huang, Director of Procedural Operations
Boston Medical Center uses the Hospital IQ platform to optimize operating room (OR) utilization. “If you’ve got ORs that are open, and you have nurses and surgical techs that are sitting around, that’s a huge wasted opportunity,” says Yi-An Huang, Director of Procedural Operations.” Hospital IQ was founded in 2013 by a team of experts in software engineering and operations science. The company’s predictive analytics platform applies research-based operations methodologies to improve hospital operational efficiency and patient quality through data-driven decision-making. “Improvements in operations help improve efficiency, quality, throughput—everything. So it’s a win-win-win,” says Krueger. Hospital IQ’s clients include Boston Medical Center, Brigham and Women’s Hospital, Thomas Jefferson University Hospitals, Greater Baltimore Medical Center, and others.
Hospital IQ currently has four modules that address a range of “pain points” experienced by hospitals and health systems:
- Surgical Planning deals with the perioperative arena, helping hospitals map out operating room usage, surgeon schedules, and related resources to predict how the OR day will come together. The platform looks at what was planned and compares it to what actually happened. This information helps the hospital to make adjustments and improve efficiency.
- Elective Smoothing looks at how the surgical schedule impacts beds in the hospital.
- Capacity Planning looks at surgical and medical demand, as well as urgent and non-urgent demand to ensure staffing is correct at various levels of care. The goal is to have the right patient in the right level of care at the right time, which positively impacts outcomes.
- Staff Scheduling helps hospitals deal with variability, which is impossible to completely eliminate. It gives them tools to automate staffing based on various factors and fine-tune as they get closer to the actual day.
“We’re very clear by module what data we need, and what we don’t need,” says Krueger. The types of data may include movement information to see how patients are moving through the system, or orders information such as orders for radiology, or for an ICU or telemetry bed. Planned and actual OR usage, staffing, and shift information, and clinical policy are other information sets that may be needed depending on the module. “It’s like Moneyball for healthcare,” says Krueger, referring to the Michael Lewis book and 2011 film based on the Oakland A’s use of data and analytics to choose players.
Boston Medical Center (BMC) piloted Hospital IQ’s Surgical Planning module in the spring of 2015, and rolled it out in the fall. BMC is a private, not-for-profit, 496-bed, academic medical center. It is the primary teaching affiliate for Boston University School of Medicine, and the largest safety net hospital in New England.
“One of the biggest challenges in terms of managing operating rooms is they’re a shared resource across different surgeons and different surgical specialties,” says Huang. “The challenge is, how much time should you be giving each surgeon, or each surgical service?” He describes common scenarios ranging from surgeons who couldn’t get their patients’ surgeries scheduled to ORs sitting vacant for a day or part of day, with allocated staff standing by with no cases.
 Prior to deploying Hospital IQ’s Surgical Planning module, Huang had been using a spreadsheet to try to understand the scheduling dynamics. “Being able to support the kinds of decisions you actually need to make was super time-consuming,” he says. “Data that is slow and hard to get is basically not data you can use.”
Prior to deploying Hospital IQ’s Surgical Planning module, Huang had been using a spreadsheet to try to understand the scheduling dynamics. “Being able to support the kinds of decisions you actually need to make was super time-consuming,” he says. “Data that is slow and hard to get is basically not data you can use.”
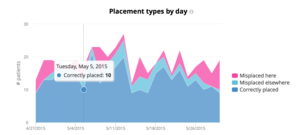
Working with Hospital IQ’s analytics platform, Huang developed tools to look at each surgical service to see whether or not surgeons were using the time blocks they had reserved, and if not, to reallocate the blocks to other surgeons that needed them. “One of the number one satisfiers for surgeons is whether they can get access to ORs,” says Huang. The tool has allowed BMC to be more responsive to surgeons, supported by data.
 From the hospital perspective, the value of full or close to full utilization of ORs is significant. “For the hospital, the amount of revenue tied to the operating rooms is tremendous,” says Huang. “If you had cases in [those empty blocks], the revenue basically drops to the bottom line.”
From the hospital perspective, the value of full or close to full utilization of ORs is significant. “For the hospital, the amount of revenue tied to the operating rooms is tremendous,” says Huang. “If you had cases in [those empty blocks], the revenue basically drops to the bottom line.”
Huang illustrates how the tool has helped him drill down to uncover surprising results. For example, orthopedics may have had 75 percent utilization of its blocks during a month. A closer look reveals certain surgeons routinely didn’t use their blocks on certain days due to conflicts in their schedules. “You should reallocate that time to somebody else,” says Huang. Although surgeons resist losing their time blocks, the data gives stakeholders transparency into what actually happened. “Having the data is huge, because otherwise it becomes a fight of anecdotes. When you have data, it becomes a lot harder to have an argument.”
Huang plans to deploy the tool in other areas such as interventional radiology and interventional cardiology. “In areas where we have a large, expensive resource that’s being shared, this tends to be an especially powerful tool,” he says.
Huang hopes to improve OR utilization by one or two percentage points, which could translate to revenue impact in the millions. “If you think about the amount of revenue you make per OR hour, it’s in the thousands of dollars,” he says. “Getting that case into existing OR time that’s been staffed is tremendously financially impactful.”
Other systems using Hospital IQ’s platform have gained insight into a range of high-impact situations.
- A hospital had higher readmissions rates for patients discharged on weekends. It turned out that the discharge process was different on weekends.
- A hospital had capacity problems at certain levels of care. They thought they needed to add more ICU beds, but the tool showed them that the bottleneck in the ICU was because there weren’t enough general beds.
- A hospital discovered that length of stay was twice as long when patients were in the wrong level of care because the staff did not have the correct skills to handle particular conditions.
 A challenge all hospitals are trying to overcome is reducing “boarding,” which is when patients are waiting in the emergency department for a bed. “If [patients] don’t get access to a bed, their length of stay goes up significantly,” says Krueger.
A challenge all hospitals are trying to overcome is reducing “boarding,” which is when patients are waiting in the emergency department for a bed. “If [patients] don’t get access to a bed, their length of stay goes up significantly,” says Krueger.
Data has great potential for helping hospitals shed light on capacity issues and understand what drives them. The benefits of solving these problems accrue to the organization as a whole as well as to individual physicians, and most of all to patients. “There’s so much data in healthcare, and I think hospital IT systems are still catching up,” says Huang. “There’s a lot of efficiency, better care, better care delivery, and design we’re just scratching the surface on right now.”
Jane Weber Brubaker is Editor of eHealthcare Strategy & Trends. Contact her at jane@ehealthcarestrategy.com.

