COVID Accelerates Enterprise Telehealth Adoption at Nemours Children’s Health
// By Marcia Simon, APR //
 The pandemic changed the dynamics of collaboration in health systems, with clinical and operations teams working side by side with marketing technology and communications departments to coordinate enterprise-wide transformation.
The pandemic changed the dynamics of collaboration in health systems, with clinical and operations teams working side by side with marketing technology and communications departments to coordinate enterprise-wide transformation.
It wasn’t just any Friday the 13th. It was March 13, 2020 — the day the federal government declared a national emergency due to the ongoing outbreak of COVID-19.
Across the country, businesses started to shut down; people started working remotely, and hospitals, including Nemours Children’s Health, had to figure out how to quickly optimize their teams to safely meet the needs of patients and providers.

Rachel Donovan, managing director of enterprise marketing strategy, Nemours Children’s Health
“I’ll never forget that day. My team was told to bring their laptops home, we trained operational support teams, ordered massive amounts of webcams, we had iPads and we were just deploying equipment everywhere. There was no formal process; it was just moving very fast,” says Rachel Donovan, managing director of enterprise marketing strategy at Nemours Children’s.
In a session at the Society for Health Care Strategy & Market Development’s SHSMD Connections 2021, “Cutting Through the Complexity of Enterprise Telehealth Adoption,” a team from Nemours Children’s shared the system’s journey and how it aligned marketing, clinical operations, and telehealth program administration to develop a cross-functional approach to transformation that met the needs of families during this critical time. Here are highlights from that presentation.
The challenge for Nemours Children’s, the largest multi-state children’s health system in the country, was unique. The system provides pediatric primary, urgent, specialty, and hospital care at two freestanding children’s hospitals and outpatient locations in Delaware, New Jersey, Pennsylvania, and Florida. With 24 hospital collaborations and 34 states leveraging Nemours Children’s evidence-based population health strategies, this wasn’t scaling an operation; it was creating a system to serve the entire enterprise.
As clinics shut down, patients, many of whom had no experience with telemedicine, needed to prepare for a new way of accessing medical visits and consultations. In one day, telemedicine went from being a small part of the larger system of care delivery to an enterprise-wide necessity to ensure patient safety.
“We trained operational support teams, ordered massive amounts of webcams, we had iPads, and we were just deploying equipment everywhere.”
Rachel Donovan
Nemours Children's Health“We had signed on with a third-party contact center prior to this and had to figure out how to train that contact center to educate families and patients who needed to get ready for a telehealth visit,” explains Donovan. The communications team wrote scripts and created ways to extract all the feedback from those calls. “We didn’t have time to think about this; we had to get information out in real time.”
Rather than convince families that “telemedicine” was the way to go, Nemours Children’s began promoting “video visits.” This language was also incorporated into display ads and campaigns for various specialties including orthopedics.
More Unexpected Challenges
Pre-COVID, about 300 Nemours Children’s providers were using telemedicine, amounting to about 10,000 virtual visits per year. In a matter of weeks, more than 1,000 providers were trained to conduct video visits, and during the peak of COVID, the system experienced an increase of 2,395% in telehealth usage, according to Susan Voltz, administrator of the telehealth program at the Center for Health Delivery Innovation at Nemours Children’s Health.
“This was fundamentally about how you learn to pivot and think about technology in a new way.”
Susan Voltz
Nemours Children's HealthVoltz, responsible for establishing and implementing the strategic direction of the enterprise telehealth program to align with the system’s overall strategies, knew that no one could have anticipated the pandemic’s power to change “the norm.” A new strategy evolved in real time, as urgency and safety became the paramount concerns.
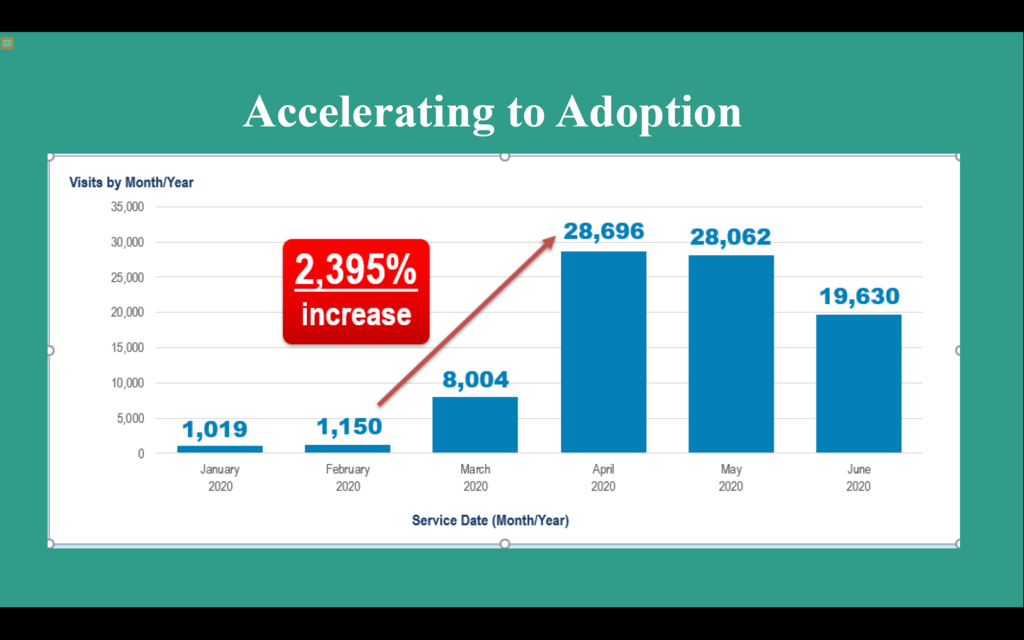
During the peak of COVID, Nemours Children’s experienced an increase of 2,395% in telehealth usage.

Susan Voltz, administrator of the Telehealth Program at the Center for Health Delivery Innovation at Nemours Children’s Health
“This was fundamentally about how you learn to pivot and think about technology in a new way,” says Voltz. Extending patient access quickly became an obvious priority. “We were familiar with video technologies, some of which — but not all — were HIPAA-compliant.”
Patients faced environments they had never experienced before, and disparities in access and platforms became clear. Delivering high-quality care to all children, regardless of location, financial status, or medical complexity, was seen as an opportunity as well as a challenge, using technology to expand this mission.
The Clinical Side
While the communications team started reaching out to patients, the challenge of onboarding physicians was managed by Patrick Barth, MD, a pediatric otolaryngologist, who serves as the system’s medical director of specialty care for telehealth.
“Providers don’t like change; they like control of their environment.”
Patrick Barth
Nemours Children's Health
Patrick Barth, MD, enterprise medical director for telehealth specialty care, Nemours Children’s Health
“Providers don’t like change; they like control of their environment,” says Barth. Even so, he says, “We lifted about 1,000 providers in about a 10-day period.”
Barth noticed that pre-COVID telemedicine barriers disappeared. “It was now a provider-driven desire to overcome the fear of technology. Primary care and specialty providers with no previous telehealth experience were suddenly looking to connect with their patients on this platform.”
This also included therapy services, lactation services, pastoral care, social work, pain management, and others. “And not just ambulatory, but also our inpatients — the children in our buildings,” says Barth. These are the kids who still needed to work with a provider, or a team of providers, while offices and remote locations experienced inconsistencies in bandwidth and Wi-Fi connections.
While hands-on care is necessary in many specialties, about 75 percent of Nemours Children’s psychology visits are still being done virtually today, after adolescent patients and their parents adjusted to the comfort and convenience of video visits.
The MarCom Strategy
As the pandemic became a reality, attending physicians at Nemours Children’s hospitals were, for the most part, eager to get trained. Reaching out to community health providers was more of a challenge, says Jenna MacPherson, marketing strategy manager at Nemours Children’s.

Jenna MacPherson, marketing strategy manager, Nemours Children’s Health
“We took a few steps forward and then a few steps back, with pushback from urgent care physicians who didn’t feel like patients would receive the same level of care,” says MacPherson. The team orchestrated a road show, visiting community health providers and get them onboard.
Nemours Children’s had the benefit of reaching communities during the pandemic through its very powerful communication tool — kidshealth.org. The world’s #1 website for trusted pediatric health information, Nemours Children’s launched the online platform in 1995 to provide physician-reviewed advice on hundreds of physical, emotional, and behavioral topics. Articles, slideshows, videos, and health tools are designed to help families learn, grow, and be their best. The site also provides free lesson plans for teachers and early-childhood educators.
“Telehealth gave us an opportunity to attract new patients.”
Jenna MacPherson
Nemours Children's HealthThe KidsHealth video production team got busy creating content to address the pandemic and educate families and community partners about video visits and the importance of continuing medical care as needed.
About six months after the initial shutdown, a patient acquisition campaign focused on differentiators to go toe-to-toe with competitors as a way to start bringing in new business.
“Telehealth gave us an opportunity to attract new patients. We found that we were holding spots open for patients who didn’t want to come in, while we tried to find available times for new patients who were eager for an office visit. We needed to address a way that was fair, with speed and intelligence, to bring people back. There was a lot of learning going on,” says MacPherson.
Hindsight 20/20
Nemours Children’s, like other hospital systems, has not settled back into “normal.” The world is still figuring out what the new normal will look like. The trend seems to be for a hybrid system that sees increased telehealth visits along with one-on-one in-person visits at the core of patient wellness and treatment. The strategy remains that the focus is always on the patient.
“Remember your intent, and remember that it’s a team effort, so share the credit when credit is due,” says Donovan. “We evolved our outreach strategy to effectively respond to changing market dynamics and always bring high-quality healthcare to our patients where and when they need it.”
Since the peak of the pandemic, Nemours Children’s has reduced the number of telehealth visits by half as patients return to the office. The pandemic has made patients and providers more comfortable with digital environments. In-person visits will never go away, but as IT and telemedicine departments analyze events of the past two years, technology’s further integration into operational and communication strategies to improve access to healthcare is waiting at the doorstep.
Marcia Simon, APR, writes about healthcare, healthtech and wellness. She manages content and strategic communication for health-based clients. Email her at marcia@mseusa.com or connect at LinkedIn.com/in/marciasimon.

