Data Management Is Key to Successful Digital Patient Initiatives
// By Ron Shinkman //
 Competent data management can be even more crucial than any specific consumer-oriented patient initiative.
Competent data management can be even more crucial than any specific consumer-oriented patient initiative.
When tasked with creating digital services to help patients find the right office or medical department at Oregon Health & Science University (OHSU) in Portland, Lisa Williams smacked right into a brick-and-mortar reality: Many buildings dotting the hospital’s sprawling, cliffside campus shared the same address as OHSU’s main hospital. That meant patients using Google Maps or relying on rideshare services could be dropped off far from the correct clinic door.

Lisa Williams, senior director of growth and loyalty at PeaceHealth
“What’s the worst thing to be doing when you don’t feel well? Being lost,” Williams said during a recent eHealthcare Strategy & Trends webinar, “Build the Data Management Foundation You Need for Successful Digital Healthcare Consumer Experiences.”
This was one of the many changes OHSU made to improve location data accuracy, working closely with the Portland Bureau of Transportation to get new and unique addresses for various buildings on its campus. The very day the new numbers were affixed to the buildings by crane, they were input into OHSU’s Google My Business profile, and then updated on Google Maps, Williams says.
Now as senior director of growth and loyalty for PeaceHealth, another large provider system in the Pacific Northwest, Williams is applying lessons from that experience to better craft digital services and platforms for patients. PeaceHealth is further challenged by its sprawling enterprise of 10 hospitals and 164 medical group offices in Alaska, Oregon, and Washington. The system treats more than 560,000 unique patients annually and has 17,000 employees.
Williams discussed her experiences along with Rachelle Montaño, vice president of clinical strategy at Loyal, an Atlanta-based technology firm that helps health systems unify enterprise data and build stronger relationships with patients by understanding their intent. It works closely with PeaceHealth on creating patient-centered digital initiatives.
A New Era For Consumer-Oriented Initiatives
Williams and Montaño are on the same page about digital initiatives to improve patient experiences: Simply plugging in service options on a website or patient portal and hoping for the best won’t work. They succeed only if the deep reservoirs of data that healthcare providers possess are carefully managed and precisely deployed.

Rachelle Montano, vice president of clinical strategy at Loyal
“Having accurate data across your enterprise is the key to success,” Montaño says.
That need for data accuracy is being driven by growing consumerism in healthcare. Patients “are really starting to exert their power more, making demands on healthcare providers, [changing the] patient relationship and really expecting to be treated much in the same way that they’re treated and doing business with any other consumer type of organization,” Montaño observes. She later added that “we’re feeling those pressures to help us find solutions” and that healthcare disruptors such as CVS Health and Amazon are putting even more pressure on providers to change.
As a result, giving patients a digital product intended to make their healthcare experiences easier should always work as advertised. And with such demands in place, competent data management can be even more crucial than any specific consumer-oriented patient initiative.
Many Data Points
That challenge is exacerbated by the huge number of data points connected to patient care. They include prior authorization referrals; online directories and scheduling; appointment management and reminders; and follow-ups and surveys, among others. And much of that data is siloed within departments that rarely communicate with one another. Or the data is embedded within different legacy systems that rarely communicate with one another.
“I know [the healthcare sector] is really tired of hearing we have stuff to learn from ecommerce, finance, and hospitality. One of the things we could do better with data is to recognize that we need to see those touchpoints cohesively,” Williams says.
A simple patient encounter may have 25 different touchpoints — both digital and non-digital — that must be appropriately aligned. They include not only looking up basic information on a medical issue but completing a request form for an appointment, researching treatment options, and even signing up for email newsletters.
Montaño acknowledges that hospital and healthcare systems can be skeptical about such initiatives. “It’s hard to develop a business case for investing in data management because data quality has no true intrinsic value,” she says. But Montaño later observed that buy-in from senior management was absolutely crucial. “This is a problem that’s much bigger than influencing the patient experience, but it’s also influencing the operation,” she says.
From the consumer side, patients and family members seeking access to cohesive information should be taken seriously by hospital and healthcare system executives at all times.
“People don’t go to our digital front doors for funsies. They’re trying to do some research because they’re sick or they have a sick [child],” Williams says. “They want to understand if you take their insurance. They want to understand if you’re the right place to help.”
And if those patients can’t get basic information such as finding the right specialists, an accurate address for where they practice, and their business hours, that’s not only going to hamstring any specific initiatives, but hamper overall digital and legacy marketing efforts, Montaño notes.
Data Management as Venn Diagram
These dynamics place successful data management smack dab in the center of a Venn diagram converging with strategy, implementation, and governance.
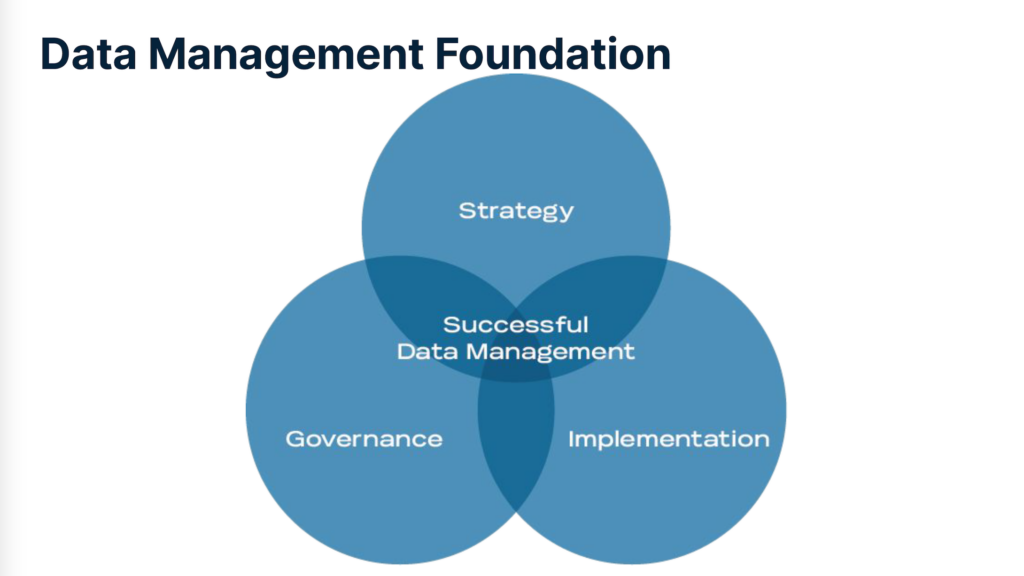
Strategy
A cohesive strategy for digital patient experience initiatives should include:
- Defining the vision and its objectives
- Identifying the resources available
- Establishing metrics for measuring success.
Governance
Governance of data management should include identifying those within an institution who manage the data; communicating to them the importance and value of data management; and identifying and recruiting stakeholders to become part of the data management process.
Formal structures should include an oversight committee to shepherd the organization toward its specific goals; a high-level executive sponsor who has enough political clout to protect initiatives and can obtain resources; and a data manager to review changes to a system’s data and receive input or suggestions for changes, among others.
Implementation
Implementation should include aligning support from stakeholders for an initiative’s goals and objectives; taking everyone’s workflow into consideration; identifying crucial data the entire institution relies on so it is properly protected; placing it into a proper taxonomic structure, and gauging the organization’s overall tolerance for disruption.
All initiatives should also have comprehensive data models and full clarification of who has stewardship over what.
The end result of such Herculean efforts? According to Williams and Montaño, when a patient is suffering from hives, their query should tell them which doctors treat hives and are accepting patients, where those doctors’ services are specifically located, where a patient can park their vehicle to receive care, and what to expect after treatment is rendered. And if a patient moves forward with seeking care, they should be provided other options such as scheduling an appointment and taking care of payments — among many others.
Unexpected Directions
Servicing those specific needs can pull a healthcare institution in unexpected directions.
One example PeaceHealth has been addressing echoes the challenge Williams faced at OHSU: The scores of clinics it has acquired over the years through mergers and acquisitions have names so disparate that the system is working on umbrella names to quell potential confusion among patients seeking care within its provider network.
“We’re going through the process of ‘How do we have a canonical name — a standard name — that gets included for every service line, every type of care center,’” Williams says. “We’re going through that right now with our operational leaders and our clinic managers to propose names for … these clinics in different communities. We’re trying to provide some standardization.” More than 40 PeaceHealth staff members from across the system were interviewed to help with the name-changing initiative.
And despite a relentless pull toward making such changes, Williams observes that healthcare organizations should not rush their patient-centered digital initiatives.
“Give yourselves grace,” she says, “and recognize that it’s going to take time to get through this process together.”
Watch the full webinar on-demand here.
Ron Shinkman is a veteran healthcare journalist. He served as West Coast Bureau Chief for Modern Healthcare and has written for a variety of other publications, including the New England Journal of Medicine publication Catalyst, Fierce Healthcare, and the Los Angeles Times. Email him at RonShinkman@gmail.com.

